E/M Hot Topic: 2022 Principal Care Management Services
Jeanie Heck, our Director of Education, wraps up our E/M Hot Topic series for 2021 discussing the new 2022 Principal Care Management Services codes. In 2022, we will have three general categories of Care Management in our E/M section. The new PCM codes allow providers, qualified health care practitioners, and clinical staff to report a code(s) for the management of a single chronic condition.
For additional information about E/M Guideline Updates education, contact us.
Follow us on LinkedIn to keep up-to-date.
In our E/M Hot Topic discussions, we previously addressed the proper capture of Social Determinant of Health (SDOH) codes that can make a difference when determining the level of service for office visit codes. When used properly, they can impact the final MDM selection and subsequent reimbursement. In the November E/M Hot Topic, Jeanie Heck, our Director of Education, re-addresses this topic and reviews the new 2022 Chapter Specific Coding Guidelines for SDOH.
For additional information about E/M Guideline Updates education, contact us.
Follow us on LinkedIn to find out when the next E/M Hot Topic is released.
In September’s E/M Hot Topic, Jeanie Heck, our Director of Education at Intellis, discusses telehealth. The 2022 Medicare Physician Fee Schedule Proposed Rule proposes that CMS allow some telehealth services to remain on the list until the end of 2023. This is intended to help determine if some of the services should be permanently added to the telehealth list following the COVID-19 PHE. During this presentation, Jeanie reviews some trustworthy and reliable sites to reference regarding telehealth.
For additional information about E/M Guideline Updates education, contact us.
Follow us on LinkedIn to find out when the next E/M Hot Topic is released.
 “Here come the ‘chart police.’”
“Here come the ‘chart police.’”
Every clinical documentation specialist (CDS) has heard it. “Chart police.” For those CDSs with a nursing background, it is often heard from those nurses they have worked alongside in the following ways:
(1) when discussing their new role
(2) while explaining their current role
(3) when attempting to recruit bedside nurses into the CDS career path.
How do we educate our bedside-loving peers about the value that their documentation brings to the final coded record? Show them.
Nurses love evidence.
It has been the foundation of nursing practice since Florence Nightingale demonstrated that good hygiene improved outcomes. Pull up a stand-alone encoder and show them the difference made by inclusion of wound staging or body mass index. Clinical documentation integrity is an obscure role to most nurses so take the opportunity to translate the language. Instead of demonstrating the MS-DRG, show the difference in severity of illness (SOI) and risk of mortality (ROM) when including their documentation. Interpreting SOI and ROM is a quicker soap box discussion than CC/MCC capture and translates clinically with almost no discussion.
ICD-10-CM Guidelines for Coding and Reporting allow us “few exceptions” to the rule that “code assignment is based on the documentation by patient’s provider” but, nurses need to know that their documentation often triggers CDSs to know that a query opportunity exists. Default templates utilized by providers may repeatedly explain that the patient is oriented, but night shift nurse documentation may paint a different picture of a sundowning patient. That picture is incredibly valuable to the accuracy of the coded record, particularly when the provider is documenting in progress notes when assessing the same patient during the day.
The remote world has done wonders for production but can put a strain on those opportunities to engage our healthcare partners and demonstrate value. Other ways to engage our nursing colleagues in understanding the value of their education: round with them during an onsite day, engage nursing management to become part of the nursing skills fairs (quality documentation is inarguably a skill), or seek out the opportunity to present to new nursing hires during orientation.
June 2021
In this month’s E/M Hot Topic, Jeanie Heck, our Director of Education, addresses some of the items from the AMA webinar on May 25th regarding the Technical Corrections published on March 9th. Many of the gray areas from the technical corrections were addressed in the AMA webinar, and she discusses some of them in her presentation.
For additional information about E/M Guideline Updates education, contact us.
Follow us on LinkedIn to find out when the next E/M Hot Topic is released.
April 2021
With the use of the 2021 E/M Guidelines, questions continue to surface. In this month’s E/M Hot Topic, Director of Education, Jeanie Heck, BBA, CCS, CPC, CRC discusses Social Determinants of Health. She also provides an update to Prescription Drug Management and the Ordering/Review of Tests.
For additional information about E/M Guideline Updates education, contact us.
Follow us on LinkedIn to find out when the next E/M Hot Topic is released.
February 2021
Now that we have been applying the new 2021 E/M guidelines for over a month, there’s no doubt that we have questions about some of the changes — especially the elements in MDM! Starting Feb 9th, Jeanie Heck, our Director of Education, will begin addressing “E/M Hot Topics” in monthly 10-20 minute presentations.
For additional information about E/M Updates education, contact us.
Coding Tip
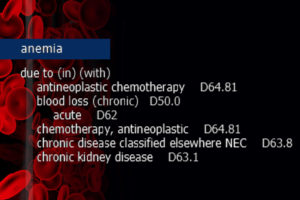
When anemia NOS is present as a current condition, and the patient has underlying chronic kidney disease (CKD) or end-stage renal disease (ESRD), it is a fast track to the usage of D63.1, Anemia in chronic kidney disease (manifestation). This is assigned unless the anemia is specified as a different form and/or attributed to another condition. Much like the diabetes category, ICD-10-CM “In/With” convention assumes “due to.”
ICD-10-CM Official Guidelines for Coding and Reporting FY 2021 Section I. A. 15.
“With”
The word “with” or “in” should be interpreted to mean “associated with” or “due to” when it appears in a code title, the Alphabetic Index (either under a main term or subterm), or an instructional note in the Tabular List. The classification presumes a causal relationship between the two conditions linked by these terms in the Alphabetic Index or Tabular List. These conditions should be coded as related even in the absence of provider documentation explicitly linking them, unless the documentation clearly states the conditions are unrelated or when another guideline exists that specifically requires a documented linkage between two conditions (e.g., sepsis guideline for “acute organ dysfunction that is not clearly associated with the sepsis”).
For conditions not specifically linked by these relational terms in the classification or when a guideline requires that a linkage between two conditions be explicitly documented, provider documentation must link the conditions in order to code them as related. The word “with” in the Alphabetic Index is sequenced immediately following the main term or subterm, not in alphabetical order.
Clinical Insight
Anemia refers to the reduction of the total number of circulating red blood cells. It is diagnosed when there is the detection of decreased hemoglobin concentration, hematocrit, or red blood cell count. Anemia in chronic kidney disease specifically falls under the category of decreased red blood cell production.
In CKD or ESRD, kidney function is compromised to the point that blood cannot be filtered of wastes and fluid. The kidneys also produce less erythropoietin (EPO), a hormone that signals the bone marrow to produce additional red blood cells. Furthermore, in CKD patients the red blood cells are not able to survive as long in the bloodstream and suffer a premature death. Due to associated nutrient deficiencies in underlying CKD, red blood cells are not reproduced as frequently or with the same cellular integrity as in a healthy patient.
Education Disclaimer: This coding tip is intended to serve the general community and may not account for all differences in coding routines, duties, or individual client policies. The information and opinions presented here are based on the experience, training, and interpretation of the author. Although the information has been researched and reviewed for accuracy, the instructor does not accept any responsibility or liability with regard to errors, omissions, misuse, or misinterpretation. This information is intended as a guide; it should not be considered a legal or consulting opinion or advice.
Intellis is pleased to announce the launch of the Intellis Intelligence Center, our innovative HIM online learning platform. We invite you to take a tour of the Intelligence Center and register to join our community of passionate educators and learners. As in introduction to online learning, we’re offering two 20-minute Coding Clinic Review courses FREE of charge. In 2018, the Intelligence Center will add dynamic training and support on a variety of topics for revenue cycle, clinical documentation improvement, and EHR professionals. We’re committed to education and leading the way in Health Information Management.

At Intellis, we’re committed to “minding the business of healthcare,” and our experts are regularly called upon to provide their insights. Recently, our VP of Education and Training, Kim Felix, RHIA, CCS, authored an article for the Healthcare Financial Management Association’s (HFMA) Revenue Cycle Strategist. The article was a Q&A piece titled “Understanding the Many Coding Changes Related to the FY18 IPPS.” The article is available to subscribers of HFMA.
Additionally, Kim has been a frequent speaker and trainer at industry events. She will be presenting an HCC Overview at the Florida Health Information Management Association (FHIMA) Coding & Clinical Documentation Institute in Orlando, Florida on February 24, 2018. In 2017, Kim spoke at a variety of events including:
PHIMA Annual Meeting
May 2017
Lancaster, PA
Overview of HCC Coding
SePHIMA Education Session
Education Committee Co-Chair
September 2017
Philadelphia, PA
FY2018 ICD-10 Coding Updates
LVHIMA Education Session
September 2017
Bethlehem, PA
FY2018 ICD-10 Coding Updates
NEPHIMA Education Session
November 2017
Wilkes Barre, PA
FY2018 ICD-10 Coding Updates
Additional articles by our HIM industry experts are available in our eNewsletter. Complete the form below to subscribe and receive information and updates or contact us for speaking engagement information.

 “Here come the ‘chart police.’”
“Here come the ‘chart police.’”