Today’s Tip: ICD-10 Anemia in CKD
Coding Tip
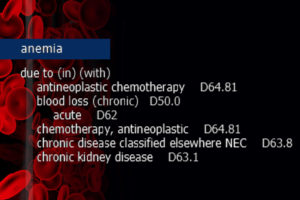
When anemia NOS is present as a current condition, and the patient has underlying chronic kidney disease (CKD) or end-stage renal disease (ESRD), it is a fast track to the usage of D63.1, Anemia in chronic kidney disease (manifestation). This is assigned unless the anemia is specified as a different form and/or attributed to another condition. Much like the diabetes category, ICD-10-CM “In/With” convention assumes “due to.”
ICD-10-CM Official Guidelines for Coding and Reporting FY 2021 Section I. A. 15.
“With”
The word “with” or “in” should be interpreted to mean “associated with” or “due to” when it appears in a code title, the Alphabetic Index (either under a main term or subterm), or an instructional note in the Tabular List. The classification presumes a causal relationship between the two conditions linked by these terms in the Alphabetic Index or Tabular List. These conditions should be coded as related even in the absence of provider documentation explicitly linking them, unless the documentation clearly states the conditions are unrelated or when another guideline exists that specifically requires a documented linkage between two conditions (e.g., sepsis guideline for “acute organ dysfunction that is not clearly associated with the sepsis”).
For conditions not specifically linked by these relational terms in the classification or when a guideline requires that a linkage between two conditions be explicitly documented, provider documentation must link the conditions in order to code them as related. The word “with” in the Alphabetic Index is sequenced immediately following the main term or subterm, not in alphabetical order.
Clinical Insight
Anemia refers to the reduction of the total number of circulating red blood cells. It is diagnosed when there is the detection of decreased hemoglobin concentration, hematocrit, or red blood cell count. Anemia in chronic kidney disease specifically falls under the category of decreased red blood cell production.
In CKD or ESRD, kidney function is compromised to the point that blood cannot be filtered of wastes and fluid. The kidneys also produce less erythropoietin (EPO), a hormone that signals the bone marrow to produce additional red blood cells. Furthermore, in CKD patients the red blood cells are not able to survive as long in the bloodstream and suffer a premature death. Due to associated nutrient deficiencies in underlying CKD, red blood cells are not reproduced as frequently or with the same cellular integrity as in a healthy patient.
Education Disclaimer: This coding tip is intended to serve the general community and may not account for all differences in coding routines, duties, or individual client policies. The information and opinions presented here are based on the experience, training, and interpretation of the author. Although the information has been researched and reviewed for accuracy, the instructor does not accept any responsibility or liability with regard to errors, omissions, misuse, or misinterpretation. This information is intended as a guide; it should not be considered a legal or consulting opinion or advice.
Keeping up with the annual updates and guidelines is a challenge for coding professionals and facility leaders. Intellis overcomes the challenge by providing tailored IQ Education that prepares coders on the frontlines to ensure their facilities are always ready for new rules.
Are you ready for October 1?
For the year 2021, ICD-10-CM official guidelines reflect over 500 significant changes. The updates include 490 new codes, 47 revised codes, and 58 codes deemed invalid. In addition, the upcoming fiscal year ICD-10-PCS code set includes 544 new codes and the recently released FY 2021 ICD-10-PCS Official Guidelines for Coding and Reporting. Effective date: October 1, 2020.
Find out more!
Right now, Intellis is offering robust training to help organizations prepare for FY 2021 ICD-10-CM, ICD-10-PCS updates. The sessions are presented by Intellis VP of Education & Training Kim Felix, RHIA, CCS a nationally recognized Intellis IQ subject matter expert.
We’re committed to helping coding teams prepare, and we provide personal service to make sure your education experience goes smoothly.
Get the details: request more info, or register now.
Contact us! We’re here to help.
As healthcare continues to evolve, more procedures and care options have moved forward in the outpatient setting. This is primarily due to technological advances and value-based care incentives.
Health insurance plans and government programs have embraced the move toward offering more services in lower-cost care settings such as outpatient facilities. As the trend toward outpatient procedures continues, what is ahead for Percutaneous Coronary Intervention? Intellis Manager of Medical Coding Integrity & Education David Steinhage RHIT, CCS examines what is on the horizon in our latest IQ Point of View.
Get the IQ Point of View: White paper – Percutaneous Coronary Intervention in the OP Setting
 COVID-19 has struck with stunning ferocity causing uncertainty across the healthcare landscape. Beyond patient care and staff safety demands, the crisis has evoked unprecedented health information challenges to medical coding and billing and clinical documentation integrity (CDI). Intellis’ immediate action continues to set the pace by providing three avenues for information and education from trusted healthcare sources and Intellis subject matter experts (SME). To date, nearly 1000 medical coders, HIM leaders, and CDI specialists along with 18 health organizations have benefited from Intellis’ commitment to sharing FREE COVID-19 educational resources.
COVID-19 has struck with stunning ferocity causing uncertainty across the healthcare landscape. Beyond patient care and staff safety demands, the crisis has evoked unprecedented health information challenges to medical coding and billing and clinical documentation integrity (CDI). Intellis’ immediate action continues to set the pace by providing three avenues for information and education from trusted healthcare sources and Intellis subject matter experts (SME). To date, nearly 1000 medical coders, HIM leaders, and CDI specialists along with 18 health organizations have benefited from Intellis’ commitment to sharing FREE COVID-19 educational resources.
One Site for Information
As the HIM industry grapples to respond and provide clear direction, ambiguity reverberated as national health organizations release evolving updates. Intellis CEO David Van Doren said, “At the outset, we recognized the huge impact of COVID-19 on health information management (HIM). With our distributed workforce, we were instantly positioned to assist providers. Further, we created our IQ Crisis Team to consolidate and share HIM information.” On the Intellis website (IntellisIQ.com), the team developed a single source where HIM professionals can obtain current COVID-19 directives and latest news from AHIMA, AMA, CDC, and CMS (intellisIQ.com/COVID-19). Each day, the website is updated as information becomes available. Also, Intellis prepared — and continually updates — Coding Tipsheets and FAQs. The Intellis IQ COVID-19 page has been visited nearly 2,500 times and the Tipsheets referenced over 1,700 times.
One Source for Online Training
To assist in disseminating timely HIM information, Intellis opened the IQ Center, the company’s education portal, to offer several FREE courses to ALL industry professionals. Intellis’ industry-recognized SMEs VP Education & Training Kim Felix, RHIA, CCS, VP of Clinical and Quality Services Allison Van Doren, RN BSN CCDS CDIP CRC, and Director of Education Jeanie Heck, BBA, CCS, CPC, CRC present coding- and CDI-related updates based on AHIMA and CMS information (education.intellisIQ.com).
One Team for COVID-19 Education
As the health crisis evolves, Intellis experts presented COVID-19 coding and CDI webinars based on AHIMA and CMS information to 18 health organizations. The one-hour sessions focused on ICD-10-CM, MS-DRG, and IP CDI updates for inpatient settings, and ICD-10-CM, CPT/HCPCS/Telemedicine, and OP CDI updates for outpatient settings. Each presentation was followed by a Q&A session. CoxHealth IP Coding Supervisor, Health Information Management Dianne Pierce, RHIT, said, “I would like to thank the Intellis educators for providing thorough, updated coding and clinical advice concerning the evolving COVID-19 pandemic. We had all of our IP and OP auditors and CDI Leadership attend at least one session and have included information we received in our policy which our coders are currently using.” Beth Israel Deaconess Medical Center (BIDMC), Director of Coding and Validation Susan B. Cohen, RHIA CDIP CCS, wrote, “Thank you so much for offering these webinars. They are so well done, and the staff really appreciate learning. Keep them coming!”
As the crisis continues, Intellis is committed to education sharing and contributing to the HIM knowledge-base. The COVID-19 online resource page, IQ Center courses, and webinars will continue to be updated as information evolves. Dates and times for updated webinars will be announced soon. Please contact info@intellisIQ.com for additional information.
# # #
About Intellis
At Intellis, our team shares a deep-rooted passion for innovation, education, and a drive to solve complex HIM challenges. With experience, best practices, and agility, we combine advisory services with flexible end-to-end solutions to address revenue cycle management and data quality issues. Our expertise improves outcomes for both providers and patients. The Intellis IQ Suite includes revenue cycle management, health information management, clinical documentation integrity (CDI), health information technology, and education and training solutions. For more information, visit www.intellisiq.com.
Media Contact:
Cassidy Communications, Inc. for Intellis
Kelly C. Vanek: 610.217.5011
kvanek@cassidycommunications.com
Our COVID-19 resources and information page is here to keep you updated on the evolving pandemic. It includes information from public health organizations, HIM organizations, and our subject matter experts intended to share HIM best practices. For education presentations and resources regarding COVID-19, please visit the Intellis IQ Center, our HIM education portal.
The Intellis IQ team of experts is ready to join your staff for an information-packed Power Hour. We dive deep into the subject matter and offer concise informational programs and presentations on a variety of timely topics tailored to select audiences and desired results.
The Intellis IQ HCC Power Hour is a comprehensive session taught by experienced presenters to address Hierarchical Condition Categories (HCC). The purpose of HCC is to enable better health management along with accurate reimbursement. To achieve the goals, coding specialists need to stay up-to-date and informed on HCC best practices. Intellis offers expert instruction with qualified presenters:
Kim Felix RHIA, CCS — Vice President of Education
Jeanie Heck BBA, CCS, CPC, CRC — Director of Education.
For more information or to schedule a “POWER HOUR” for your team, please contact Intellis President Dan Cooke.
Should organizations address stigmatizing language in medical records?
That is the question posed by Lisa A. Eramo, MA in her article “Choose Your Words Carefully” in a recent edition of For The Record. “Words matter. It’s not only what you write but also how you write it that affects others. This is true in a variety of settings, and health care is certainly no exception. In fact, a recent study conducted by researchers at Johns Hopkins University School of Medicine (Journal of General Internal Medicine, May 2018) found that the words providers document in patients’ medical records affect how other clinicians perceive and ultimately care for those patients—and not necessarily for the better.
‘I think sometimes we consider the medical record as a collection of objectively recorded data and plans, but when you step back, it becomes clear that you can really shape the narrative about a patient in very different ways, both implicitly and explicitly,” says Anna Goddu, MD, lead author and a medical student at Johns Hopkins University.’ ”
For real-world insight into how word usage and stigmatizing language in patient health records affect provider perception, Eramo tapped Intellis HCC experts Kim Felix, RHIA, CCS, vice president of education and training and Jeanie Heck, CCS, CPC, CRC, director of education. Kim addressed examples of stigmatizing language. Further, she supported creating an atmosphere where CDI specialist feel safe flagging stigmatizing language and alerting risk management or quality assurance. Jeanie addressed the need to maintain professionalism and emphasized mandatory education to ensure less experienced staff understand the importance of appropriate language.
The full article is available in For the Record.
Recently, our VP of Coding Operation Darina Kutish, RHIT, CCS provided expert insight to For The Record magazine’s feature “Of Viral Importance” written by Lisa A. Eramo, MA.
Of Viral Importance
Why Your Hospital’s Reputation Depends—at Least Partially—on Accurate Pneumonia Coding
These days, it takes seconds for patients to view mortality and readmissions data on the Centers for Medicare & Medicaid Services’ Hospital Compare website (www.medicare.gov/hospitalcompare). With a few clicks of the mouse, they can—and frequently do—draw conclusions about the quality of care that’s provided.
Pneumonia, which causes approximately 1 million hospital admissions annually, according to the Centers for Disease Control and Prevention, is one of several diagnoses listed on Hospital Compare. Coded data are what drives these publicly reported quality measures, making it imperative that organizations undertake a concerted effort to correctly capture diagnostic specificity and sequence conditions.
All cases with a principal diagnosis of pneumonia are included in the 30-day risk-standardized pneumonia readmission measure as well as the 30-day risk-standardized pneumonia mortality measure. Cases with a principal diagnosis of sepsis (with the exception of severe sepsis) and a secondary diagnosis of pneumonia coded as present on admission (POA) are also included in these measures when there is no additional secondary diagnosis of severe sepsis (ie, R65.20 [severe sepsis without septic shock] or R65.21 [severe sepsis with septic shock]) coded as POA.
“The bottom line is that all pneumonia codes are on the hook for mortality and readmissions,” says James P. Fee, MD, CCS, CCDS, CEO of Enjoin. “Aspiration pneumonia used to be the only one that was excluded, but now it’s also included.”
(For a complete list of ICD-10-CM codes as well as inclusion/exclusion criteria and risk adjustment for both pneumonia measures, visit the QualityNet website at www.qualitynet.org.)
Hospitals need to understand that these data drive consumer decisions about where to receive health care services, says Dee Mandley, RHIT, CCS, CCS-P, CDIP, lead educator at Peak Health Solutions. “Anyone can go on this site and compare hospitals based on pneumonia information, so you need to make sure that it’s coded correctly.”
In addition to quality measure implications, pneumonia coding affects reimbursement and length of stay. For example, unspecified pneumonia maps to diagnosis-related group (DRG) 195 (simple pneumonia and pleurisy without complication or comorbidity [CC] or major CC [MCC]) with a relative weight of 0.6868 and 2.6-day geometric length of stay. The more specific aspiration and certain specified bacterial pneumonias both map to DRG 179 (respiratory infections and inflammations without CC/MCC) with a relative weight of 0.9215 and 3.2-day geometric length of stay.
When reported as a secondary diagnosis, pneumonia carries an MCC status and can have a positive effect on the final Medicare severity DRG (MS-DRG) assignment, Mandley says. Pneumonia also carries a severity of illness rating of three and a risk of mortality rating of two, both of which have a positive effect on all patient refined DRG assignment, she adds.
Documentation Challenges
When it comes to accurate pneumonia coding, conflicting documentation is one of the biggest challenges for coders, says Darina Kutish, RHIT, CCS, vice president of coding operations at Intellis. “Some doctors will call it pneumonia, some will call it an infiltrate based on the X-ray, and some may say bronchitis. The documentation makes some of these cases very difficult to code.”
Coders must recognize clinical indicators of pneumonia and query when necessary, Kutish says. For example, symptoms such as fever, cough, shortness of breath, pleuritic chest pain, and respiratory distress can be clues that pneumonia is present. Other clues include a physical exam that shows rails, rhonchi, and abnormal breath sounds. The patient may also have an elevated white blood cell count and a chest X-ray showing consolidation, an infiltrate, and/or interstitial changes. Finally, the sputum culture may be positive for an organism.
“These are all good clinical indicators to back up the pneumonia. The sputum cultures do not need to be positive, but if they are, it can help support a query,” Kutish says.
According to Mandley, another challenge is identifying the principal diagnosis when the patient has multiple pulmonary conditions on admission such as respiratory failure, COPD, and pneumonia. Coders must think carefully when assigning pneumonia as the principal diagnosis because doing so means the case will potentially be included in the 30-day readmission and mortality measures. When in doubt, a query to the physician is necessary, Mandley says.
When multiple conditions are POA and all meet the definition of principal diagnosis, coders have the flexibility to choose the diagnosis that will yield the highest-weighted DRG, Kutish says. The principal diagnosis is defined in the Uniform Hospital Discharge Data Set as “that condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care.” For example, when pneumonia and acute respiratory failure are both POA and meet the definition of principal diagnosis, coders can report the pneumonia as the principal diagnosis with acute respiratory failure as a secondary MCC.
Scenario-Specific Pneumonia Coding Tips
Experts say pneumonia can present in many different ways; the clinical circumstances of each case will drive ICD-10-CM code assignment and sequencing. The following are several common scenarios with tips for compliant coding.
Unspecified Pneumonia
Coders should report ICD-10-CM code J18.9 when the cause of pneumonia is unknown. This can occur when sputum cultures are negative. Coders should also report J18.9 when physicians document one of the following conditions: community-acquired pneumonia, hospital-acquired pneumonia, or health care–acquired pneumonia, Mandley says.
Sputum cultures may be negative when patients receive antibiotics upon admission to the hospital and before cultures are taken or when the quality of the specimen is lacking, she adds. They may also be negative when patients are already on an antibiotic for another condition such as a urinary tract infection.
However, coders should always perform a thorough review of the record rather than default to an unspecified type, says Regina Jackson, CPC, CPMA, CPC-I, co-owner at EnR Coding Solutions. Doing so presents a more accurate clinical picture of severity of illness and risk of mortality, she says.
Pneumonia as a Manifestation of an Infectious Disease
When influenza causes pneumonia, coders should report a code from the ICD-10-CM J09.- through J11.- range. When the type of influenza is known—and physicians link the influenza with the pneumonia—report combination codes J09.- or J10.-. When the type of influenza is not known, report J11.-, says Elizabeth Hankins, CPC, CCS-P, CPMA, CPC-I, PMCC, co-owner and founder of EnR Coding Solutions.
Remember that patients can have more than one type of pneumonia simultaneously (eg, pneumonia due to influenza and pneumonia due to a bacterium). “You have to really carefully review the documentation on admission to see where the bulk of treatment is going,” Mandley says.
When coding tuberculosis that causes pneumonia, refer to the key term “pneumonia” in the alphabetic index and then the subterm “tuberculosis,” which directs coders to see “tuberculosis, pulmonary.” Thus, ICD-10-CM code A15.0 (tuberculosis of lung, including tuberculosis pneumonia) is appropriate, says Mary Frungillo-Tomak, CCS, CDIP, manager of inpatient coding, clinical documentation improvement (CDI) audit, and education at Atos.
Aspiration Pneumonia
Coders should report ICD-10-CM code J69.0 for aspiration pneumonia and be prepared to query physicians in the absence of explicit documentation when clinical indicators of aspiration pneumonia are present, according to Kutish. These include poststroke dysphagia and reflux disease as well as a swallowing study to assess the patient’s gag reflex or the presence of a nasogastric tube, she adds.
Bacterial Pneumonia
When there’s a positive sputum culture, physicians should link the specific organism causing the pneumonia so coders can choose the appropriate ICD-10-CM code for the bacterial pneumonia, Kutish says. “The doctor has to state the significance of that positive culture. If they don’t state that significance, then you cannot report the more specific code,” she explains.
The following is a sample statement that would allow coders to report ICD-10 code J15.5: “Patient has positive sputum culture for E coli and we’re treating them for E coli pneumonia.”
Mandley reminds coders to keep in mind that the type of bacterial organism can affect the final MS-DRG assignment. For example, gram-negative pneumonia maps to ICD-10-CM code J15.6, driving a respiratory infection DRG. Pneumonia due to Streptococcus pneumoniae maps to ICD-10-CM code J13, driving a lower-weighted simple pneumonia DRG.
Pneumonia That Causes Sepsis
When sepsis and pneumonia are both POA, coders should assign the sepsis as the principal diagnosis and the localized infection (pneumonia) as secondary per official coding guidelines, Frungillo-Tomak says.
These guidelines state: “If the reason for admission is both sepsis or severe sepsis and a localized infection, such as pneumonia or cellulitis, a code(s) for the underlying systemic infection should be assigned first and the code for the localized infection should be assigned as a secondary diagnosis. If the patient has severe sepsis, a code from subcategory R65.2 should also be assigned as a secondary diagnosis. If the patient is admitted with a localized infection, such as pneumonia, and sepsis/severe sepsis doesn’t develop until after admission, the localized infection should be assigned first, followed by the appropriate sepsis/severe sepsis codes.”
Pneumonia Due to Near Drowning
When a patient has pneumonia due to near drowning, coders should refer to the Excludes 1 note under ICD-10-CM code T75.1xx- (unspecified effects of drowning and nonfatal submersion) that instructs coders to code to the specified effects of the drowning (ie, pneumonia, J18.9), Kutish says.
Pneumonia With Acute Exacerbation of COPD
This situation requires the following codes: J44.0 (COPD with acute lower respiratory infection), J18.9 (pneumonia, unspecified organism), and J44.1 (COPD with acute exacerbation). Previously, J44.0 had a “use additional code” note to identify the infection, meaning coders were required to report the pneumonia code as a secondary diagnosis.
“Now there is a ‘code also’ note that does not denote sequencing. Therefore, you may sequence either one as the principal diagnosis depending on the circumstances of the admission,” Kutish says.
Tips to Promote Pneumonia Data Integrity
Experts share the following tips to ensure that coded data reflect pneumonia specificity:
• Provide coder education. Recruit a physician champion to educate coders about the types of pneumonia as well as causes, risk factors, signs, symptoms, complications, and treatment, Mandley says.
“Without knowledge of the disease, a coder is unable to analyze the clinical documentation in the medical record and recognize the need for a physician query to capture specificity of the diagnosis,” Frungillo-Tomak says. “It’s also necessary to compose a compliant query.”
• Provide physician education. A physician champion can educate physicians about pneumonia documentation requirements such as causative organisms, pneumonia type, and any associated conditions (eg, acute exacerbation of COPD and the presence of influenza), Mandley says.
“For inpatients, documentation of possible or probable diagnoses infers a strong clinical suspicion and can be coded as present,” she notes, adding it’s a good idea to incorporate documentation education into the orientation schedule for new residents and to post documentation tips and fliers in patient care areas.
• Use denials as teaching tools. Ask coders and CDI staff to review these cases so they understand why denials occur and how to prevent them proactively, Mandley says. For example, payers may assign a lower-weighted DRG if the POA indicator for the pneumonia is incorrect (ie, reported as Y when it should have been N).
Some payers may also deny pneumonia when the chest X-ray is negative, making it critical to document and code all of the patient’s other pneumonia symptoms, Kutish notes. “Get that bulletproof documentation up front so payers can’t deny payment,” she says.
• Analyze pneumonia queries. Do coders and CDI specialists frequently query one or two physicians? Or do queries tend to address the same documentation problem across the board? “A CDI program can provide tremendous data for analyzing coding and documentation patterns,” Mandley says.
• Develop clinical indicators. Mandley recommends involving medical staff in identifying specific clinical indicators that CDI and coding staff can use when assessing the presence of pneumonia.
• Promote collaboration between coding and CDI. Consider scheduling a recurring meeting so staff can discuss diagnoses that the organization may be struggling to report correctly, Frungillo-Tomak says.
She says these meetings are ideal opportunities to do the following:
— Exchange knowledge. CDI specialists can provide clinical education on pneumonia to coders, and coders can educate CDI staff on the application of pneumonia-related coding guidelines and Coding Clinic quarterly updates.
— Review and standardize physician queries to reflect specific types of pneumonia.
— Use a standardized dispute process to discuss cases for which coders and CDI specialists disagreed on final DRG assignment.
“I think it’s important for coders, CDI specialists, and physicians to work together to get that documentation so you get the most accurate payment for the hospital,” Kutish says.
— Lisa A. Eramo, MA, is a freelance writer and editor in Cranston, Rhode Island, who specializes in HIM, medical coding, and health care regulatory topics.
The For the Record feature “Of Viral Importance” was included with permission. Copyright © 2019.

At Intellis, we’re committed to “minding the business of healthcare,” and our experts are regularly called upon to provide their insights. Recently, our VP of Education and Training, Kim Felix, RHIA, CCS, authored an article for the Healthcare Financial Management Association’s (HFMA) Revenue Cycle Strategist. The article was a Q&A piece titled “Understanding the Many Coding Changes Related to the FY18 IPPS.” The article is available to subscribers of HFMA.
Additionally, Kim has been a frequent speaker and trainer at industry events. She will be presenting an HCC Overview at the Florida Health Information Management Association (FHIMA) Coding & Clinical Documentation Institute in Orlando, Florida on February 24, 2018. In 2017, Kim spoke at a variety of events including:
PHIMA Annual Meeting
May 2017
Lancaster, PA
Overview of HCC Coding
SePHIMA Education Session
Education Committee Co-Chair
September 2017
Philadelphia, PA
FY2018 ICD-10 Coding Updates
LVHIMA Education Session
September 2017
Bethlehem, PA
FY2018 ICD-10 Coding Updates
NEPHIMA Education Session
November 2017
Wilkes Barre, PA
FY2018 ICD-10 Coding Updates
Additional articles by our HIM industry experts are available in our eNewsletter. Complete the form below to subscribe and receive information and updates or contact us for speaking engagement information.
