Immunodeficiency Status Codes
 New codes were created in October 2020 to report specific causes for a patient’s immunocompromised state. Previously, there was no way to capture a patient who was immunocompromised or immunodeficient. The only way was to use the “long-term use of drugs” and/or the conditions related to the immunocompromised state.
New codes were created in October 2020 to report specific causes for a patient’s immunocompromised state. Previously, there was no way to capture a patient who was immunocompromised or immunodeficient. The only way was to use the “long-term use of drugs” and/or the conditions related to the immunocompromised state.
So what does it mean when a patient is immunocompromised or immunodeficient?
An immunocompromised state refers to the weakened condition of an individual’s immune system that makes it less able to fight infections and other diseases. When the immune system fails to respond adequately to infection, it’s called an immunodeficiency, and the patient may become immunocompromised.
Treating a patient who is immunocompromised poses more risks and challenges; therefore, it is important to identify a patient with this status whether coding hospital Inpatient/Outpatient or Physician Office records.
Why is this important for coding?
The new D codes below are all Complications/Comorbidities (CCs) that will impact the MS-DRG for inpatient reimbursement. And they also have an effect on Risk Adjustment Scores for Medicare Advantage patients since these codes are CMS-HCCs (Hierarchical Condition Categories).
Multiple codes may be assigned to show immunodeficiency due to multiple causes (e.g., cancer and antineoplastic medication). In cases where the cause of the immunosuppression is not clearly documented, query the provider.
D84.821 Immunodeficiency due to drugs
Immunodeficiency due to medications that interfere with the immune system. These medications include but are not limited to immunosuppressants, corticosteroids and chemotherapy.
D84.822 Immunodeficiency due to external causes
Immunodeficiency caused by external factors such as exposure to radiation therapy or due to bone marrow transplant.
D84.81 Immunodeficiency due to conditions classified elsewhere
Created for an immunocompromised state due to a specific medical condition such as HIV, AIDS*,(See explanation below) certain cancers and genetic disorders that are classified elsewhere in ICD-10-CM.
D84.89 Other immunodeficiencies
*There was an update in the First Quarter 2021 Coding Clinic that clarified the use of D84.81. “It is not appropriate to assign code D84.81, Immunodeficiency due to conditions classified elsewhere, together with code B20, human immunodeficiency virus (HIV) disease. Immunocompromise/immunodeficiency is part of the clinical picture in HIV disease, and code B20 captures fully the immunocompromised state.” Fortunately, there is an Excludes1 note under code D84.81, excluding B20, confirming that HIV/AIDS is not coded here.
Here are some examples of the new Immunodeficiency Status codes in practical use directly from Coding Clinic:
Question:
A patient was seen in the emergency department for cellulitis of two fingers on her right hand. She was admitted to start intravenous antibiotics due to having an immunocompromised state caused by immunosuppressant medication that she takes for systemic lupus erythematosus (SLE). What are the appropriate code assignments for the admission?
Answer:
Assign code L03.011, Cellulitis of the right finger, as the principal diagnosis. Assign codes M32.9, Systemic lupus erythematosus, unspecified, for SLE, D84.821, Immunodeficiency due to drugs, and Z79.899, Other long-term (current) drug therapy, for the patient’s immunosuppressed state due to long-term use of immunosuppressants.
In this case, the immunosuppressant medication was prescribed by the provider to suppress the patient’s immune system. An adverse effect code is not assigned when the medication has achieved its intended result in lowering the patient’s immune response to systemic lupus erythematosus.
Question:
A patient with multiple myeloma was seen for ear pain and cold symptoms due to acute otitis media of the left ear and acute viral bronchitis. The provider documented that the patient is immunosuppressed due to current long-term chemotherapy. What are the appropriate code assignments for this encounter?
Answer:
Sequence either code J20.8, Acute bronchitis due to other specified organisms, or code H66.92, Otitis media, unspecified, left ear, as the first-listed diagnosis. Assign codes D84.821, Immunodeficiency due to drugs, for the patient’s immunosuppressed state as a result of chemotherapy, and T45.1X5A, Adverse effect of antineoplastic and immunosuppressive drugs, initial encounter. In this case, immune suppression is not part of the intended effect of the antineoplastic drugs and is coded as an adverse effect. Additionally, assign codes C90.00, Multiple myeloma not having achieved remission, for the multiple myeloma and Z79.899, Other long term (current) drug therapy, for the chemotherapy.
Measuring body mass index (BMI)requires the following equation:
BMI = (weight (lb) ÷ height2 (in)) x 703
 The Result?
The Result?
BMI = A physiologically misleading indicator used to classify health status. Misleading because weight divided by height squared (x 703 to make up for the metric system) tells us nothing about a patient’s bone density or muscle mass, both of which tell us a great deal about a person’s physical health. This misleading indicator is then broken into categories that patients are often bucketed into: underweight (below 18.5), normal (18.5-24.9), overweight (25.0-29.9), obese (30.0-39.9), morbidly obese (over 40) without consideration of gender, ethnicity, age, or athleticism variances. Well-conditioned athletes and weightlifters often have notoriously high BMI’s due to exceptional bone health and increased muscle mass.
Clinical Significance
Coding Clinic addresses in Fourth Quarter 2018 that “obesity and morbid obesity are always clinically significant and reportable when documented by the provider. In addition, if documented, the body mass index (BMI) code may be coded in addition to the obesity or morbid obesity code.” But what happens when the provider has not documented a diagnosis? One cannot assume the clinical significance of a number without an associated diagnosis. Without more information about a patient, we cannot be sure that the elevated BMI requires a diagnosis or is simply a numerical finding without clinical relevance because the patient is a world-renowned bodybuilder.
An Inherent Issue
Clinical documentation integrity (CDI) specialists and coders are often trained to look for the BMI and the accompanying appearance of an associated diagnosis when a high or low value is noted. There is an inherent issue in this practice. Recall the inpatient guidelines for reporting additional diagnoses (Section III. Reporting Additional Diagnoses: General Rules for Other (Additional) Diagnoses):
“For reporting purposes, the definition for ‘other diagnoses’ is interpreted as additional conditions that affect patient care in terms of requiring: clinical evaluation; or therapeutic treatment; or diagnostic procedures; or extended length of hospital stay; or increased nursing care and/or treatment.”
The burden of proof rests on the CDI specialist or coder to demonstrate that a condition met “other” diagnosis criteria yet was not documented when initiating a query. Aside from being a questionable result to a math equation, how did the patient’s elevated or low BMI impact their hospital stay?
Many CDI specialists default back to “weight-based medications.” Can you identify the weight-based medications in a patient who did not receive anesthesia? Every nurse took a course in medication math to get through nursing school. If your patient received a heparin infusion at a weight-based dose, did a weight of 285 pounds in a 5’5” patient impact nursing care more than a weight of 285 pounds in a 6’5” patient would have when calculating a dose? There is an argument for therapeutic treatment varying but before you ask the question, be sure your argument is sound.
Indicators
There are indicators to look for that justify that some BMI-related diagnoses may be clinically significant. Read the nurse’s notes. Fully dependent or even partially dependent patients requiring “max assist” or “OOB w/ assist x2” demonstrates that additional nursing care was required. Specialty beds come at a premium and provide support to patients above and beyond that of a traditional inpatient bed. Nutrition consults to help a patient with a BMI of 17.0 gain weight are obviously targeted treatment.
Be on the lookout for “other” reasons for inaccurate BMI and avoid falling into the traps. Patients and clinicians are usually not accurate when guessing a patient’s weight. If you see a solid even number (say 300 pounds) entered into the electronic medical record, do some digging to see “how” the patient was weighed. Standing scales and bed scales are far more accurate than “self-report.” While it seems very specific, be mindful of bilateral amputees. Most electronic records automatically calculate BMI based on the input height and weight. Any amputee requires special consideration for the percentage of body surface lost.
Performing the CDI role is to assess a patient without the use of your senses. For those with a clinical background that required patient assessment, the CDI role requires that you do the same assessment without ever seeing, touching, or hearing the patient. Querying for accuracy in the patient record takes unique skills and it is important to exercise those skills prudently when attempting to assess a patient with a potentially misleading number.
Need help keeping your Coding and CDI teams up-to-date? Contact us to find out how we can help. Intellis offers in-depth education and training services led by our IQ Team of subject matter experts.
April 2021
With the use of the 2021 E/M Guidelines, questions continue to surface. In this month’s E/M Hot Topic, Director of Education, Jeanie Heck, BBA, CCS, CPC, CRC discusses Social Determinants of Health. She also provides an update to Prescription Drug Management and the Ordering/Review of Tests.
For additional information about E/M Guideline Updates education, contact us.
Follow us on LinkedIn to find out when the next E/M Hot Topic is released.
Since we have passed the one-year anniversary that COVID-19 was first identified in the United States, it is important to reflect on the long-term effects of COVID-19. Throughout the pandemic, the Intellis team has worked diligently to update COVID-19 resources. Research continues to evolve as the medical community seeks to better understand the disease’s impact, and the passage of time presents the opportunity to evaluate the effects on body systems.
According to the Journal of the American Medical Association, the pandemic has been accompanied by a COVID-19 “infodemic” with more than 11,000 COVID-19 papers submitted to JAMA since the start of the pandemic! It can be overwhelming to keep up. Our White Papers serve as a guide to remind coders and clinical documentation integrity (CDI) specialists to dig deeper into the medical record to uncover overlooked diagnosis documentation. The goal is to highlight some, but not all, of the commonly seen complications in the patient population infected with COVID-19.
White Paper: Sequelae of COVID-19 Part I – Cardiac, Pulmonary, Dermatological Complications
White Paper: Sequelae of COVID-19: Part II – Neurological, Psychological, Renal complications
The ICD-10-CM code for Chronic Kidney Disease (CKD) Stage 3 (N18.3) has been revised for Fiscal Year 2021. The most recent update to the CMS-HCC Risk Adjustment Model has CKD Stage 3 making an impact on Risk Adjustment Factor scores. On the other hand, CKD Stage 3 is not recognized as a complication or comorbidity (CC) in the DRG world of coding.
Not only do the new codes for CKD Stage 3 give more specificity and capture more detail, but they also help to define more precisely the edge within Stage 3 at which mortality becomes the main concern.
The new codes are as follows:
- N18.30 CKD, Stage 3 unspecified
- N18.31 CKD, Stage 3a (GFR = 45-59)
- N18.32 CKD, Stage 3b (GFR= 30-44)
Kidney disease is often asymptomatic and occurs just before kidney failure. About one-third of the population of older adults have CKD Stage 3. When someone is experiencing Stage 3, it means their kidneys are filtering about half of what they should be, allowing for some fluids, electrolytes, and waste to build up in the body.
CKD often starts to develop without notice. However, symptoms may appear in Stage 3. For those that do experience symptoms, these may include fatigue, swelling around the ankles or eyes, unusually light-colored urine, urinating more frequently, and loss of appetite.
Once an individual has Stage 3 CKD, it’s generally considered to be irreversible. Fortunately, the majority of Stage 3 patients do not progress to the more severe stages. Still, it is important to work with a doctor to manage the condition and gain a clear picture in regard to the GFR and kidneys. This helps to identify the need for kidney replacement therapy sooner and essentially helps to keep the patient healthier longer.
References:
https://www.fairview.org/blog/A-Third-of-Older-Adults-have-Stage-3-Chronic-Kidney-Disease
March 2021
As we continue to use the new 2021 E/M Guidelines, many questions continue to surface. In this month’s E/M Hot Topic, Director of Education, Jeanie Heck, BBA, CCS, CPC, CRC discusses the review and/or ordering of tests, independent interpretation of tests, and discussion of management or test interpretation from the data element of MDM.
For additional information about E/M Guideline Updates education, contact us.
The April 2021 E/M Hot Topic: Social Determinants of Health
Follow us on LinkedIn to find out when the next E/M Hot Topic is released.
“1 in 2 people with very low kidney function who are not on dialysis do not know they have CKD (chronic kidney disease).” — Center for Disease Control
The implications of untreated or unmanaged kidney disease can be life-altering or lethal. CKD is a manageable co-morbid condition in its early stages with the potential for reversibility, however, once chronic kidney disease hits the later stages, management of the disease becomes significantly more resource consumptive. CMS is now in line with the clinical information by updating the most recent version of their HCC’s to reflect that even moderate CKD impacts the patient’s risk.
The intention of hierarchical condition category (HCC) coding is to utilize the patient’s medical conditions, demographics, and interactions of the patient’s diseases to calculate a risk adjustment factor (RAF) score. The RAF score conveys the severity of the patient’s conditions in a calendar year in an attempt to reflect the level of resource consumption required to manage the patient. Anyone assigning diagnosis codes, regardless of setting, should be aware and educated on this risk-based payment methodology.
Inpatient care, awareness of kidney function matters for the management of other disease processes and medications. In coding, the accuracy of appropriate staging does not just impact the care rendered. Accuracy also ensures that the patient’s RAF score accurately reflects the resource consumption of their disease process. Through code assignment and documentation, the diagnosis can be linked to those underlying conditions that most often cause degradation of the kidneys- hypertension, and diabetes.
In earlier versions of CMS-HCCs, CKD did not carry significant risk (as demonstrated through weight) until the patient’s disease had reached stages 4, 5, or end-stage renal disease. In this case, the eGFR (estimated glomerular filtration rate) has typically dropped below 30, demonstrating a serious impact on the ability to clear waste products from the bloodstream.
CKD stage 3 (eGFR typically ranging 30-59) was not recognized as a hierarchical condition category code. This changed, however, with the introduction of CMS-HCC version 24. Why the change? CKD stage 3 (N18.30) has clinically significant ramifications for comorbid disease management and medication usage. Treating and managing a patient with CKD stage 3 before progression to later stages has a significant impact on the health of the patient. CMS did not outright make this statement but it’s a clinically logical deduction from the understanding of CKD disease progression.
In the inpatient setting, CKD stage 3 is not recognized as a complication or comorbidity (CC) so clinical documentation specialists may be overlooking this important risk adjusting condition. It is important that whether functioning in the inpatient or outpatient setting, CDI specialists and coders focus on getting accurate information reflecting the patient’s health status documented in the medical record. Take a deep look at the details of the patient encounter next time “CKD, unspecified” (N18.9) appears in the record.
Wondering about those more specific CKD stage 3 codes? Look for more information regarding CKD stages 3a and 3b in future tips!
February 2021
Now that we have been applying the new 2021 E/M guidelines for over a month, there’s no doubt that we have questions about some of the changes — especially the elements in MDM! Starting Feb 9th, Jeanie Heck, our Director of Education, will begin addressing “E/M Hot Topics” in monthly 10-20 minute presentations.
For additional information about E/M Updates education, contact us.
Coding Tip
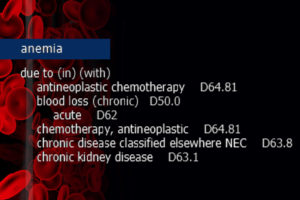
When anemia NOS is present as a current condition, and the patient has underlying chronic kidney disease (CKD) or end-stage renal disease (ESRD), it is a fast track to the usage of D63.1, Anemia in chronic kidney disease (manifestation). This is assigned unless the anemia is specified as a different form and/or attributed to another condition. Much like the diabetes category, ICD-10-CM “In/With” convention assumes “due to.”
ICD-10-CM Official Guidelines for Coding and Reporting FY 2021 Section I. A. 15.
“With”
The word “with” or “in” should be interpreted to mean “associated with” or “due to” when it appears in a code title, the Alphabetic Index (either under a main term or subterm), or an instructional note in the Tabular List. The classification presumes a causal relationship between the two conditions linked by these terms in the Alphabetic Index or Tabular List. These conditions should be coded as related even in the absence of provider documentation explicitly linking them, unless the documentation clearly states the conditions are unrelated or when another guideline exists that specifically requires a documented linkage between two conditions (e.g., sepsis guideline for “acute organ dysfunction that is not clearly associated with the sepsis”).
For conditions not specifically linked by these relational terms in the classification or when a guideline requires that a linkage between two conditions be explicitly documented, provider documentation must link the conditions in order to code them as related. The word “with” in the Alphabetic Index is sequenced immediately following the main term or subterm, not in alphabetical order.
Clinical Insight
Anemia refers to the reduction of the total number of circulating red blood cells. It is diagnosed when there is the detection of decreased hemoglobin concentration, hematocrit, or red blood cell count. Anemia in chronic kidney disease specifically falls under the category of decreased red blood cell production.
In CKD or ESRD, kidney function is compromised to the point that blood cannot be filtered of wastes and fluid. The kidneys also produce less erythropoietin (EPO), a hormone that signals the bone marrow to produce additional red blood cells. Furthermore, in CKD patients the red blood cells are not able to survive as long in the bloodstream and suffer a premature death. Due to associated nutrient deficiencies in underlying CKD, red blood cells are not reproduced as frequently or with the same cellular integrity as in a healthy patient.
Education Disclaimer: This coding tip is intended to serve the general community and may not account for all differences in coding routines, duties, or individual client policies. The information and opinions presented here are based on the experience, training, and interpretation of the author. Although the information has been researched and reviewed for accuracy, the instructor does not accept any responsibility or liability with regard to errors, omissions, misuse, or misinterpretation. This information is intended as a guide; it should not be considered a legal or consulting opinion or advice.
Keeping up with the annual updates and guidelines is a challenge for coding professionals and facility leaders. Intellis overcomes the challenge by providing tailored IQ Education that prepares coders on the frontlines to ensure their facilities are always ready for new rules.
Are you ready for October 1?
For the year 2021, ICD-10-CM official guidelines reflect over 500 significant changes. The updates include 490 new codes, 47 revised codes, and 58 codes deemed invalid. In addition, the upcoming fiscal year ICD-10-PCS code set includes 544 new codes and the recently released FY 2021 ICD-10-PCS Official Guidelines for Coding and Reporting. Effective date: October 1, 2020.
Find out more!
Right now, Intellis is offering robust training to help organizations prepare for FY 2021 ICD-10-CM, ICD-10-PCS updates. The sessions are presented by Intellis VP of Education & Training Kim Felix, RHIA, CCS a nationally recognized Intellis IQ subject matter expert.
We’re committed to helping coding teams prepare, and we provide personal service to make sure your education experience goes smoothly.
Get the details: request more info, or register now.
Contact us! We’re here to help.
Partnership supports highly accurate patient matching and patient record management for providers as they implement new EHR platforms
At Intellis, we’re trusted industry experts offering customized and flexible revenue cycle management services for hospitals and health systems. We’re proud to enhance our efforts with a new partner. We’re teaming with Verato a leading provider of cloud-based identity resolution services. Together we’re enabling customers to leverage integrated technology and services. This ensures accurate matching of patient medical and financial records with the right patient.
Behind the numbers
A Pew Trust research analysis found that when healthcare organizations do not have the right capabilities in place for patient matching, the resulting errors have a significant impact on patient safety and healthcare costs:
- One in five hospital chief information officers links an instance of patient harm to a mismatch in patient records.
- Up to half of patient records are not accurately matched during transfers from one facility to another, such as from a rural hospital to an urban facility.
- Up to one in five patient records within the same health system are not accurately matched with patients.
Sometimes, these errors are due to typos made while inputting patient information during registration. Also, patient information changes, data formatting issues, and insurance fraud are culprits. Mismatched records are expensive to fix: One hospital spent $96 per patient record to resolve duplicate records in its system.
President’s perspective
“The partnership between Intellis and Verato increases efficiency in EHR consolidation. Also, it aids clinicians at the point of care when the ability to access the right information quickly is critical to providing trusted care,” says Dan Cooke, President, Intellis. “We’re pleased to partner with Verato in providing state-of-the-art solutions for seamless integration and migration of EHRs. Our joint “services plus solutions” approach protects the integrity of patient data as well as patient safety.”
Our COVID-19 coding and CDI education and training webinars are AHIMA-Approved for CEUs. We are constantly focused on COVID-19 coding and CDI, and we’re quick to recognize and share critical changes as they become available. Our FREE education and training webinars are led by the Intellis IQ team of subject matter experts. The information presented is based on trusted healthcare sources including the American Health Information Management Association (AHIMA), the American Medical Association (AMA), the Centers for Disease Control and Prevention (CDC), and the Centers for Medicare & Medicaid Services (CMS). The education presented is monitored continuously to reflect the most current healthcare and industry updates.
Schedule your FREE live webinars today!
Email our Intellis IQ Team
For information call: 484.264.1609
Each webinar includes a 1-hour education session presented by the Intellis IQ team of industry experts. Download the webinar overview or view below.

 The Result?
The Result?