Today’s Tip: Hypercholesterolemia and Hyperlipidemia
 Providers often use the terms hyperlipidemia and hypercholesterolemia interchangeably. Technically, hyperlipidemia is a high or elevated lipid/fat level in the blood. High blood cholesterol is a lipid disorder. As a result, when hyperlipidemia and hypercholesterolemia are both documented in the record, only assign code E78.00 (Pure hypercholesterolemia) per Coding Clinic, Second Quarter 2022. On the other hand, when ‘mixed hyperlipidemia’ and ‘hypercholesterolemia’ are both documented, assign code E78.2 (Mixed hyperlipidemia). In this example, hypercholesterolemia is included in the E78.2 code.
Providers often use the terms hyperlipidemia and hypercholesterolemia interchangeably. Technically, hyperlipidemia is a high or elevated lipid/fat level in the blood. High blood cholesterol is a lipid disorder. As a result, when hyperlipidemia and hypercholesterolemia are both documented in the record, only assign code E78.00 (Pure hypercholesterolemia) per Coding Clinic, Second Quarter 2022. On the other hand, when ‘mixed hyperlipidemia’ and ‘hypercholesterolemia’ are both documented, assign code E78.2 (Mixed hyperlipidemia). In this example, hypercholesterolemia is included in the E78.2 code.
M&A Overview
Last year, President Joe Biden ordered the FTC and other federal agencies to promote market
competition in healthcare. Biden said hospital mergers and acquisitions had left the 10 largest
healthcare systems in control of a quarter of the market and led to the closure of hospitals in
rural and other underserved areas.
Yet even as antitrust enforcement builds, total revenue from hospital and health system
mergers and acquisitions (M&A) during the second quarter of 2022 far exceeded that of any
prior year’s second quarter, according to Kaufman Hall’s latest industry report. Some of the
largest healthcare systems are happy to merge. Or they’re buying up surgery centers,
independent practices, and more.
“Provider M&A is here to stay.”
John Lynn, blogger, Health IT Today
The Kaufman report predicts a couple of reasons for the uptick. Hospitals need to find partners
that can help them continue to evolve, including growth in outpatient services, telehealth
programs, and home healthcare. And, smaller hospitals that face financial challenges may see
it’s no longer viable to stay independent and may need partners.
Shifts in healthcare delivery, regulation, and expectations of providers can create both
opportunities and constraints when it comes to IT infrastructure during M&A. From security
risks to duplicate medical records, here are five important IT considerations during the process.
Three IT Considerations During M&A
1. Ensure IT Has a Voice During Due Diligence
M&A transactions require a thorough evaluation of complex IT requirements to encourage data sharing, pinpoint cost savings, and increase clinical value. While CIOs and IT leaders have gained a seat at the table during the due diligence process over the past few years, hard lessons are learned if IT is not part of early discussions. Thorough assessments of IT infrastructure, network capabilities, data centers, and more are required. This ensures a solid understanding of the applications environment and IT staffing requirements, which reduces unnecessary financial, technical, and security risks.
2. Conduct Security Risk Assessments
Introducing new business partners or taking part in a merger or acquisition comes with new security risks that must be considered. Ferdinand Hamada, managing director of healthcare at MorganFranklin Cyber, predicts that a high volume of M&A activity will continue into the rest of 2022, and he encourages healthcare organizations to conduct thorough risk assessments and make sure that new business partners are aligned with the organization’s existing security processes and controls.
3. Prioritize Master Patient Index Cleanup
The sheer complexity of migrating millions of patient records from multiple EHRs into a new system can’t be overlooked. A master patient index (MPI) cleanup strategy to tackle all disparate systems and duplicate patient information across facilities is crucial. In fact, when done right, this endeavor enhances patient identity integrity, care delivery, and revenue cycle activities. Case in point: A NJ-based health system that underwent a combination of different M&As over seven years was tasked with migrating Epic into 14 hospitals and 1,000 providers. The consolidation happened over time, where multiple organizations came together and made for a challenging situation. There were nine different EHR systems and approximately 650 downstream systems, including labs, radiology, respiratory, and more. After thorough planning, the health network’s team embarked on the formidable task of migrating 8.3 million patient records from multiple EHRs to the new system. You can learn more about this project here.
Keep IT Agile During M&A
With no end in sight to M&A activity, it is imperative that CIOs and IT leaders get involved early
on to plan for the situations listed above. Keeping information systems agile, adaptable,
efficient, and powerful across healthcare organizations is essential. Click here to learn how
Intellis can support MPI cleanup and more.
By Glenn Schweidler, RHIA
Chief Operations Officer and Partner
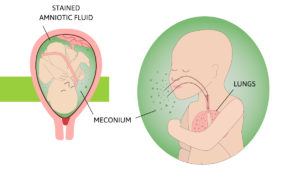 Meconium gives the amniotic fluid a greenish color. This is called meconium staining. Coding Clinic, Second Quarter 2022 clarifies ‘light meconium-stained fluid’ and how to code it. The presence of any meconium staining may indicate fetal distress, therefore code O77.0 (Labor and delivery affected by meconium in amniotic fluid) is appropriate to code if documented as such. There does not need to be documentation of fetal distress or maternal conditions to code.
Meconium gives the amniotic fluid a greenish color. This is called meconium staining. Coding Clinic, Second Quarter 2022 clarifies ‘light meconium-stained fluid’ and how to code it. The presence of any meconium staining may indicate fetal distress, therefore code O77.0 (Labor and delivery affected by meconium in amniotic fluid) is appropriate to code if documented as such. There does not need to be documentation of fetal distress or maternal conditions to code.
2022 ICD-10-CM CODE O77.0
 Eliquis can be used as an anticoagulant or an antithrombotic. When a patient is on Eliquis long-term, it can be a coding conundrum. As published in Coding Clinic, Second Quarter 2022, ICD-10-CM classifies Eliquis as an anticoagulant medication. Therefore, if long-term use of Eliquis is documented in the record, assign code Z79.01 (The long-term (current) use of anticoagulants).
Eliquis can be used as an anticoagulant or an antithrombotic. When a patient is on Eliquis long-term, it can be a coding conundrum. As published in Coding Clinic, Second Quarter 2022, ICD-10-CM classifies Eliquis as an anticoagulant medication. Therefore, if long-term use of Eliquis is documented in the record, assign code Z79.01 (The long-term (current) use of anticoagulants).
 This condition is commonly documented along with chronic kidney disease (CKD). MBD is a broad term used to describe a group of bone disorders of bone strength usually caused by mineral abnormalities such as calcium, phosphorus, vitamin D, or magnesium. As published in Coding Clinic, Second Quarter 2022, when MBD is a component of another disease process, only the underlying condition (e.g., secondary hyperparathyroidism or renal osteodystrophy) is coded. If no underlying condition is documented, code the appropriate code from subcategory M89.8X-.
This condition is commonly documented along with chronic kidney disease (CKD). MBD is a broad term used to describe a group of bone disorders of bone strength usually caused by mineral abnormalities such as calcium, phosphorus, vitamin D, or magnesium. As published in Coding Clinic, Second Quarter 2022, when MBD is a component of another disease process, only the underlying condition (e.g., secondary hyperparathyroidism or renal osteodystrophy) is coded. If no underlying condition is documented, code the appropriate code from subcategory M89.8X-.
Following Oracle’s $28.4 billion acquisition of Cerner Corporation, board chair and CTO Larry Ellison announced his vision of a national health records database. Health IT Answers reached out to Intellis Chief Operations Officer Glenn Schweidler, RHIA, and other industry leaders to find out what they think about developing a national health records database. https://www.healthitanswers.net/leaders-weigh-in-on-oracle-acquisition-and-new-vision/
 When Lupus (unspecified) is documented in a record, there is no default code. Therefore, it is important to have providers document this condition as precisely as possible.
When Lupus (unspecified) is documented in a record, there is no default code. Therefore, it is important to have providers document this condition as precisely as possible.
For instance, document SLE (systemic lupus erythematosus) instead and add any complications that accompany this diagnosis. It is often accompanied by Sjogren’s syndrome or Sicca syndrome, which have very specific codes. Another solution is to develop facility or provider-specific guidelines to report M32.9 (SLE, unspecified) as a default for Lupus, unspecified.

Intellis is pleased to announce the addition of Lori Harbison, LPN, CCDS, CDIP, CCS as our Manager of Clinical Documentation and Quality Services.
Lori brings over 30 years of experience in nursing, including 13 years of experience in Clinical Documentation Integrity. A proven subject matter expert with a deep understanding of review, audit, and education, Lori is respected for her contributions and vast knowledge in the Clinical Documentation field.
Lori is a credentialed CDI specialist holding a CDIP from AHIMA and a CCDS from ACDIS. Additionally, Lori is a clinical LPN and credentialed CCS. Lori’s philosophy is built on the principle that to meaningfully affect clinical documentation, the physician, CDS, and coder must work together as a cohesive unit. She is committed and passionate about fostering and advancing physician engagement and clinical documentation integrity education. Lori has developed and presented customized education programs for individual physicians, large-scale physician groups, and health care systems, which has driven increased physician engagement and quality documentation. Lori is recognized for the advancement of the CDI profession by her work on many innovative targeted projects, including early adoption of CDI at patient round table discussions and CDI discussion at physician rounding and other progressive initiatives.
Prior to joining Intellis, Lori led the CDI training program at the Cleveland Clinic for 13 years. As the Quality and Education Coordinator, Lori was charged with the comprehensive training of clinical nurses, coders, and HIM professionals in their complete education as CDI specialists. In this capacity, she developed detailed training programs and continuing education for the growth and development of skilled and experienced CDI specialists. Lori is an accomplished educator and mentor with a proven record of successfully training adult learners. Lori prides herself on the long-term accomplishments of her trainees, many of whom hold CDI leadership positions as well as other health care executive roles.
Certifications
- Certified Clinical Documentation Specialist (CCDS)
- Certified Clinical Documentation Practitioner (CDIP)
- Certified Coding Specialist (CCS)
- Licensed Practical Nurse (LPN)
Industry Areas
- Inpatient clinical documentation integrity
- Clinical documentation education-physician
- Clinical documentation education-CDI specialist
- Medical Record Review and Auditing
- Query compliance
- Inpatient Coding
# # #
Media Contact:
Dan Cooke, President
 Drug-induced neuropathy (D62.0) is a diagnosis often missed by even the savviest and seasoned coders. It is sometimes seen in documentation as ‘CIPN’ (chemotherapy-induced peripheral neuropathy) and is a common side effect caused by antineoplastic agents. Treatment includes steroids and nerve pain medication such as Gabapentin.
Drug-induced neuropathy (D62.0) is a diagnosis often missed by even the savviest and seasoned coders. It is sometimes seen in documentation as ‘CIPN’ (chemotherapy-induced peripheral neuropathy) and is a common side effect caused by antineoplastic agents. Treatment includes steroids and nerve pain medication such as Gabapentin.
Drugs related to neuropathy
The most likely chemotherapy drugs related to neuropathy include platinum drugs, such as oxaliplatin; taxanes, such as docetaxel; vinca alkaloids, such as vincristine; and myeloma treatments, such as bortezomib. This code can also be accompanied by another code for the adverse effect (T36-T50) to identify the drug.
For March 2022, our IN THE KNOW newsletter focuses on:
-
Ransomware Recovery
• Earning CEUs
• Employment Opportunities
• Welcoming Elaine Lips
• Coding Tips

Intellis is honored to announce the addition of Elaine Lips, RHIA, SHIMSS as Business Development Strategist to support company growth ambitions and client expansion initiatives in the Western Region of the U.S.
“I’m pleased and inspired to join Intellis to expand their western region client presence.” — Elaine Lips, RHIA, SHIMSS
An innovator with an entrepreneurial spirit, Elaine comes to Intellis with over 40 years of experience in healthcare consulting and information services. She has owned two successful national Health Information Management (HIM)/Mid Revenue Cycle consulting firms. She has held various leadership roles, including strategic business planning, development, operational management using best practices, clinical documentation improvement, and mid revenue cycle outsourcing.
Elaine is an Advanced Member of the Healthcare Financial Management Association (HFMA) and Senior Member of the Health Information Management Systems Society (HIMSS). Further, she has been active with the American Health Information Management Association (AHIMA), and she was elected and served on the California Health Information Association (CHIA) board of directors.
Currently serving on the Editorial Board for HcPRO’s HIM Briefings, Elaine is a frequent speaker and author. She was the recipient of AHIMA’s Visionary Award and CHIA’s Industry Champion award.
Elaine’s proactive approach, respected thought leadership, extensive client development experience, and strong communication skills will help drive innovation and fuel our growth through client expansion as she begins her partnership with Intellis.
# # #
Media Contact:
Dan Cooke, President
 Cachexia (R64) is also known as ‘wasting’ or ‘wasting syndrome’. It is a general state of weakness involving marked weight and muscle loss. Emaciated is another term that may be found in the documentation that also maps to code R64.
Cachexia (R64) is also known as ‘wasting’ or ‘wasting syndrome’. It is a general state of weakness involving marked weight and muscle loss. Emaciated is another term that may be found in the documentation that also maps to code R64.
These diagnoses are often missed since they are commonly only seen in the Physical Exam or Review of Systems portion of a record. There are often ‘knee-jerk’ reactions that can lead a coder to investigate further if a patient may have these diagnoses.
What to look for
Cachexia is commonly seen in patients who have AIDS, cancer, or other advanced heart or lung disease. You will often see a lack of appetite, fatigue, low BMI, and malnutrition. Look for nutritional consults and a PEG tube in the documentation to trigger the search for cachexia in the documentation.
Why is this so important?
Cachexia is a diagnosis that can affect reimbursement for both Inpatient and Risk Adjustment. Don’t miss it!