E/M Hot Topic: Takeaways from AMA’s 5/25 Webinar on E/M Office Visit Technical Corrections
June 2021
In this month’s E/M Hot Topic, Jeanie Heck, our Director of Education, addresses some of the items from the AMA webinar on May 25th regarding the Technical Corrections published on March 9th. Many of the gray areas from the technical corrections were addressed in the AMA webinar, and she discusses some of them in her presentation.
For additional information about E/M Guideline Updates education, contact us.
Follow us on LinkedIn to find out when the next E/M Hot Topic is released.
 New codes were created in October 2020 to report specific causes for a patient’s immunocompromised state. Previously, there was no way to capture a patient who was immunocompromised or immunodeficient. The only way was to use the “long-term use of drugs” and/or the conditions related to the immunocompromised state.
New codes were created in October 2020 to report specific causes for a patient’s immunocompromised state. Previously, there was no way to capture a patient who was immunocompromised or immunodeficient. The only way was to use the “long-term use of drugs” and/or the conditions related to the immunocompromised state.
So what does it mean when a patient is immunocompromised or immunodeficient?
An immunocompromised state refers to the weakened condition of an individual’s immune system that makes it less able to fight infections and other diseases. When the immune system fails to respond adequately to infection, it’s called an immunodeficiency, and the patient may become immunocompromised.
Treating a patient who is immunocompromised poses more risks and challenges; therefore, it is important to identify a patient with this status whether coding hospital Inpatient/Outpatient or Physician Office records.
Why is this important for coding?
The new D codes below are all Complications/Comorbidities (CCs) that will impact the MS-DRG for inpatient reimbursement. And they also have an effect on Risk Adjustment Scores for Medicare Advantage patients since these codes are CMS-HCCs (Hierarchical Condition Categories).
Multiple codes may be assigned to show immunodeficiency due to multiple causes (e.g., cancer and antineoplastic medication). In cases where the cause of the immunosuppression is not clearly documented, query the provider.
D84.821 Immunodeficiency due to drugs
Immunodeficiency due to medications that interfere with the immune system. These medications include but are not limited to immunosuppressants, corticosteroids and chemotherapy.
D84.822 Immunodeficiency due to external causes
Immunodeficiency caused by external factors such as exposure to radiation therapy or due to bone marrow transplant.
D84.81 Immunodeficiency due to conditions classified elsewhere
Created for an immunocompromised state due to a specific medical condition such as HIV, AIDS*,(See explanation below) certain cancers and genetic disorders that are classified elsewhere in ICD-10-CM.
D84.89 Other immunodeficiencies
*There was an update in the First Quarter 2021 Coding Clinic that clarified the use of D84.81. “It is not appropriate to assign code D84.81, Immunodeficiency due to conditions classified elsewhere, together with code B20, human immunodeficiency virus (HIV) disease. Immunocompromise/immunodeficiency is part of the clinical picture in HIV disease, and code B20 captures fully the immunocompromised state.” Fortunately, there is an Excludes1 note under code D84.81, excluding B20, confirming that HIV/AIDS is not coded here.
Here are some examples of the new Immunodeficiency Status codes in practical use directly from Coding Clinic:
Question:
A patient was seen in the emergency department for cellulitis of two fingers on her right hand. She was admitted to start intravenous antibiotics due to having an immunocompromised state caused by immunosuppressant medication that she takes for systemic lupus erythematosus (SLE). What are the appropriate code assignments for the admission?
Answer:
Assign code L03.011, Cellulitis of the right finger, as the principal diagnosis. Assign codes M32.9, Systemic lupus erythematosus, unspecified, for SLE, D84.821, Immunodeficiency due to drugs, and Z79.899, Other long-term (current) drug therapy, for the patient’s immunosuppressed state due to long-term use of immunosuppressants.
In this case, the immunosuppressant medication was prescribed by the provider to suppress the patient’s immune system. An adverse effect code is not assigned when the medication has achieved its intended result in lowering the patient’s immune response to systemic lupus erythematosus.
Question:
A patient with multiple myeloma was seen for ear pain and cold symptoms due to acute otitis media of the left ear and acute viral bronchitis. The provider documented that the patient is immunosuppressed due to current long-term chemotherapy. What are the appropriate code assignments for this encounter?
Answer:
Sequence either code J20.8, Acute bronchitis due to other specified organisms, or code H66.92, Otitis media, unspecified, left ear, as the first-listed diagnosis. Assign codes D84.821, Immunodeficiency due to drugs, for the patient’s immunosuppressed state as a result of chemotherapy, and T45.1X5A, Adverse effect of antineoplastic and immunosuppressive drugs, initial encounter. In this case, immune suppression is not part of the intended effect of the antineoplastic drugs and is coded as an adverse effect. Additionally, assign codes C90.00, Multiple myeloma not having achieved remission, for the multiple myeloma and Z79.899, Other long term (current) drug therapy, for the chemotherapy.
Measuring body mass index (BMI)requires the following equation:
BMI = (weight (lb) ÷ height2 (in)) x 703
 The Result?
The Result?
BMI = A physiologically misleading indicator used to classify health status. Misleading because weight divided by height squared (x 703 to make up for the metric system) tells us nothing about a patient’s bone density or muscle mass, both of which tell us a great deal about a person’s physical health. This misleading indicator is then broken into categories that patients are often bucketed into: underweight (below 18.5), normal (18.5-24.9), overweight (25.0-29.9), obese (30.0-39.9), morbidly obese (over 40) without consideration of gender, ethnicity, age, or athleticism variances. Well-conditioned athletes and weightlifters often have notoriously high BMI’s due to exceptional bone health and increased muscle mass.
Clinical Significance
Coding Clinic addresses in Fourth Quarter 2018 that “obesity and morbid obesity are always clinically significant and reportable when documented by the provider. In addition, if documented, the body mass index (BMI) code may be coded in addition to the obesity or morbid obesity code.” But what happens when the provider has not documented a diagnosis? One cannot assume the clinical significance of a number without an associated diagnosis. Without more information about a patient, we cannot be sure that the elevated BMI requires a diagnosis or is simply a numerical finding without clinical relevance because the patient is a world-renowned bodybuilder.
An Inherent Issue
Clinical documentation integrity (CDI) specialists and coders are often trained to look for the BMI and the accompanying appearance of an associated diagnosis when a high or low value is noted. There is an inherent issue in this practice. Recall the inpatient guidelines for reporting additional diagnoses (Section III. Reporting Additional Diagnoses: General Rules for Other (Additional) Diagnoses):
“For reporting purposes, the definition for ‘other diagnoses’ is interpreted as additional conditions that affect patient care in terms of requiring: clinical evaluation; or therapeutic treatment; or diagnostic procedures; or extended length of hospital stay; or increased nursing care and/or treatment.”
The burden of proof rests on the CDI specialist or coder to demonstrate that a condition met “other” diagnosis criteria yet was not documented when initiating a query. Aside from being a questionable result to a math equation, how did the patient’s elevated or low BMI impact their hospital stay?
Many CDI specialists default back to “weight-based medications.” Can you identify the weight-based medications in a patient who did not receive anesthesia? Every nurse took a course in medication math to get through nursing school. If your patient received a heparin infusion at a weight-based dose, did a weight of 285 pounds in a 5’5” patient impact nursing care more than a weight of 285 pounds in a 6’5” patient would have when calculating a dose? There is an argument for therapeutic treatment varying but before you ask the question, be sure your argument is sound.
Indicators
There are indicators to look for that justify that some BMI-related diagnoses may be clinically significant. Read the nurse’s notes. Fully dependent or even partially dependent patients requiring “max assist” or “OOB w/ assist x2” demonstrates that additional nursing care was required. Specialty beds come at a premium and provide support to patients above and beyond that of a traditional inpatient bed. Nutrition consults to help a patient with a BMI of 17.0 gain weight are obviously targeted treatment.
Be on the lookout for “other” reasons for inaccurate BMI and avoid falling into the traps. Patients and clinicians are usually not accurate when guessing a patient’s weight. If you see a solid even number (say 300 pounds) entered into the electronic medical record, do some digging to see “how” the patient was weighed. Standing scales and bed scales are far more accurate than “self-report.” While it seems very specific, be mindful of bilateral amputees. Most electronic records automatically calculate BMI based on the input height and weight. Any amputee requires special consideration for the percentage of body surface lost.
Performing the CDI role is to assess a patient without the use of your senses. For those with a clinical background that required patient assessment, the CDI role requires that you do the same assessment without ever seeing, touching, or hearing the patient. Querying for accuracy in the patient record takes unique skills and it is important to exercise those skills prudently when attempting to assess a patient with a potentially misleading number.
Need help keeping your Coding and CDI teams up-to-date? Contact us to find out how we can help. Intellis offers in-depth education and training services led by our IQ Team of subject matter experts.
The ICD-10-CM code for Chronic Kidney Disease (CKD) Stage 3 (N18.3) has been revised for Fiscal Year 2021. The most recent update to the CMS-HCC Risk Adjustment Model has CKD Stage 3 making an impact on Risk Adjustment Factor scores. On the other hand, CKD Stage 3 is not recognized as a complication or comorbidity (CC) in the DRG world of coding.
Not only do the new codes for CKD Stage 3 give more specificity and capture more detail, but they also help to define more precisely the edge within Stage 3 at which mortality becomes the main concern.
The new codes are as follows:
- N18.30 CKD, Stage 3 unspecified
- N18.31 CKD, Stage 3a (GFR = 45-59)
- N18.32 CKD, Stage 3b (GFR= 30-44)
Kidney disease is often asymptomatic and occurs just before kidney failure. About one-third of the population of older adults have CKD Stage 3. When someone is experiencing Stage 3, it means their kidneys are filtering about half of what they should be, allowing for some fluids, electrolytes, and waste to build up in the body.
CKD often starts to develop without notice. However, symptoms may appear in Stage 3. For those that do experience symptoms, these may include fatigue, swelling around the ankles or eyes, unusually light-colored urine, urinating more frequently, and loss of appetite.
Once an individual has Stage 3 CKD, it’s generally considered to be irreversible. Fortunately, the majority of Stage 3 patients do not progress to the more severe stages. Still, it is important to work with a doctor to manage the condition and gain a clear picture in regard to the GFR and kidneys. This helps to identify the need for kidney replacement therapy sooner and essentially helps to keep the patient healthier longer.
References:
https://www.fairview.org/blog/A-Third-of-Older-Adults-have-Stage-3-Chronic-Kidney-Disease
March 2021
As we continue to use the new 2021 E/M Guidelines, many questions continue to surface. In this month’s E/M Hot Topic, Director of Education, Jeanie Heck, BBA, CCS, CPC, CRC discusses the review and/or ordering of tests, independent interpretation of tests, and discussion of management or test interpretation from the data element of MDM.
For additional information about E/M Guideline Updates education, contact us.
The April 2021 E/M Hot Topic: Social Determinants of Health
Follow us on LinkedIn to find out when the next E/M Hot Topic is released.
“1 in 2 people with very low kidney function who are not on dialysis do not know they have CKD (chronic kidney disease).” — Center for Disease Control
The implications of untreated or unmanaged kidney disease can be life-altering or lethal. CKD is a manageable co-morbid condition in its early stages with the potential for reversibility, however, once chronic kidney disease hits the later stages, management of the disease becomes significantly more resource consumptive. CMS is now in line with the clinical information by updating the most recent version of their HCC’s to reflect that even moderate CKD impacts the patient’s risk.
The intention of hierarchical condition category (HCC) coding is to utilize the patient’s medical conditions, demographics, and interactions of the patient’s diseases to calculate a risk adjustment factor (RAF) score. The RAF score conveys the severity of the patient’s conditions in a calendar year in an attempt to reflect the level of resource consumption required to manage the patient. Anyone assigning diagnosis codes, regardless of setting, should be aware and educated on this risk-based payment methodology.
Inpatient care, awareness of kidney function matters for the management of other disease processes and medications. In coding, the accuracy of appropriate staging does not just impact the care rendered. Accuracy also ensures that the patient’s RAF score accurately reflects the resource consumption of their disease process. Through code assignment and documentation, the diagnosis can be linked to those underlying conditions that most often cause degradation of the kidneys- hypertension, and diabetes.
In earlier versions of CMS-HCCs, CKD did not carry significant risk (as demonstrated through weight) until the patient’s disease had reached stages 4, 5, or end-stage renal disease. In this case, the eGFR (estimated glomerular filtration rate) has typically dropped below 30, demonstrating a serious impact on the ability to clear waste products from the bloodstream.
CKD stage 3 (eGFR typically ranging 30-59) was not recognized as a hierarchical condition category code. This changed, however, with the introduction of CMS-HCC version 24. Why the change? CKD stage 3 (N18.30) has clinically significant ramifications for comorbid disease management and medication usage. Treating and managing a patient with CKD stage 3 before progression to later stages has a significant impact on the health of the patient. CMS did not outright make this statement but it’s a clinically logical deduction from the understanding of CKD disease progression.
In the inpatient setting, CKD stage 3 is not recognized as a complication or comorbidity (CC) so clinical documentation specialists may be overlooking this important risk adjusting condition. It is important that whether functioning in the inpatient or outpatient setting, CDI specialists and coders focus on getting accurate information reflecting the patient’s health status documented in the medical record. Take a deep look at the details of the patient encounter next time “CKD, unspecified” (N18.9) appears in the record.
Wondering about those more specific CKD stage 3 codes? Look for more information regarding CKD stages 3a and 3b in future tips!
February 2021
Now that we have been applying the new 2021 E/M guidelines for over a month, there’s no doubt that we have questions about some of the changes — especially the elements in MDM! Starting Feb 9th, Jeanie Heck, our Director of Education, will begin addressing “E/M Hot Topics” in monthly 10-20 minute presentations.
For additional information about E/M Updates education, contact us.
Coding Tip
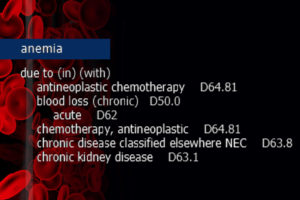
When anemia NOS is present as a current condition, and the patient has underlying chronic kidney disease (CKD) or end-stage renal disease (ESRD), it is a fast track to the usage of D63.1, Anemia in chronic kidney disease (manifestation). This is assigned unless the anemia is specified as a different form and/or attributed to another condition. Much like the diabetes category, ICD-10-CM “In/With” convention assumes “due to.”
ICD-10-CM Official Guidelines for Coding and Reporting FY 2021 Section I. A. 15.
“With”
The word “with” or “in” should be interpreted to mean “associated with” or “due to” when it appears in a code title, the Alphabetic Index (either under a main term or subterm), or an instructional note in the Tabular List. The classification presumes a causal relationship between the two conditions linked by these terms in the Alphabetic Index or Tabular List. These conditions should be coded as related even in the absence of provider documentation explicitly linking them, unless the documentation clearly states the conditions are unrelated or when another guideline exists that specifically requires a documented linkage between two conditions (e.g., sepsis guideline for “acute organ dysfunction that is not clearly associated with the sepsis”).
For conditions not specifically linked by these relational terms in the classification or when a guideline requires that a linkage between two conditions be explicitly documented, provider documentation must link the conditions in order to code them as related. The word “with” in the Alphabetic Index is sequenced immediately following the main term or subterm, not in alphabetical order.
Clinical Insight
Anemia refers to the reduction of the total number of circulating red blood cells. It is diagnosed when there is the detection of decreased hemoglobin concentration, hematocrit, or red blood cell count. Anemia in chronic kidney disease specifically falls under the category of decreased red blood cell production.
In CKD or ESRD, kidney function is compromised to the point that blood cannot be filtered of wastes and fluid. The kidneys also produce less erythropoietin (EPO), a hormone that signals the bone marrow to produce additional red blood cells. Furthermore, in CKD patients the red blood cells are not able to survive as long in the bloodstream and suffer a premature death. Due to associated nutrient deficiencies in underlying CKD, red blood cells are not reproduced as frequently or with the same cellular integrity as in a healthy patient.
Education Disclaimer: This coding tip is intended to serve the general community and may not account for all differences in coding routines, duties, or individual client policies. The information and opinions presented here are based on the experience, training, and interpretation of the author. Although the information has been researched and reviewed for accuracy, the instructor does not accept any responsibility or liability with regard to errors, omissions, misuse, or misinterpretation. This information is intended as a guide; it should not be considered a legal or consulting opinion or advice.

 The Result?
The Result?